SICKLE CELL AND BLOOD EXCHANGE
Life-changing Sickle Cell Disease treatment approved by NHS watchdog
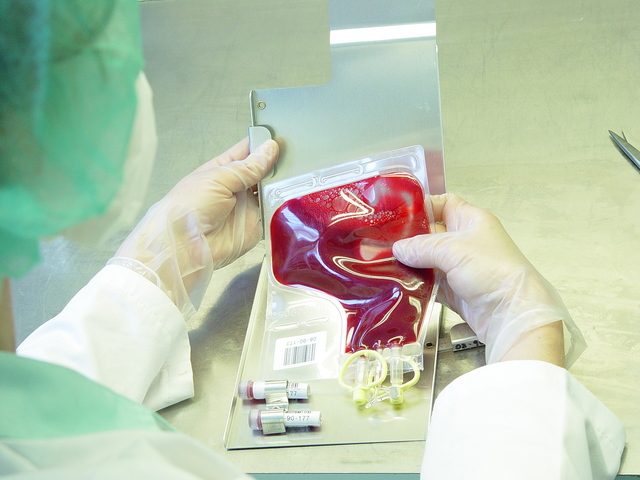
A new automatic blood transfusion treatment will half the number of visits to hospital for people with Sickle Cell Disease
Thousands of people suffering from Britain’s most common genetic disorder have been offered new hope after the health watchdog approved a ground-breaking new treatment.
Sickle Cell Disease affects around 15,000 people in Britain who struggle to make enough red blood cells to carry oxygen around the body.
Current treatments involve lengthy manual transfusions which can take more than 24 hours every month. But a new device allows the red blood cells to be replaced in as little as three hours, and patients need only visit a clinic for the therapy six times a year.
“Treatments are very limited, so this new guidance recommends a novel option which is very good news for patients as it makes the red blood cell exchange process faster and less frequent. The device could save the NHS in England an estimated £13 million each year – around £18,000 per patient – with the size of the saving depending on the patient’s condition and the equipment already owned by the NHS.”
In sickle cell disease, blood cells are a crescent – or sickle – shape instead of the normal round disc shape, affecting the cell’s ability to carry oxygen and move around the body.
Symptoms may include intense pain and severe anaemia, and the condition can cause damage to major organs and infections, and life-threatening complications. There is no cure for sickle cell disease but patients can be supported to manage the condition.
Currently blood transfusion therapies increase the amount of iron in a person’s body which can lead to serious problems such as liver disease or heart failure. Iron limiting therapy is required to reduce the amount of iron in the body, but this treatment can make some patients feel unwell and is very expensive for the NHS.
John James, Chief Executive of the Sickle Cell Society, said: “The Sickle Cell Society welcomes the NICE guidance on Spectra Optia.
“The Society has worked hard to improve access to this technology, and participated in the process every step of the way with NICE to help produce the guidance.
“Many people living with sickle cell would benefit from automated red cell exchange and guidance will enable more and more patients to access this treatment. We anticipate that this guidance will help more hospitals adopt the technology, saving patients from costly and often exhausting travel.”
http://www.telegraph.co.uk






Having read this I believed it was really enlightening. I appreciate you spending some time and effort to put this content together. I once again find myself spending a lot of time both reading and commenting. But so what, it was still worthwhile!
http://helpfultip.eu
Many thanks for your comments and wishing you well.
I visit day-to-day a few websites and information sites to read posts, except this blog provides feature based writing.
http://financehints.eu
Many thanks for your comments, do keep visiting and wish you well.
I couldn’t resist commenting. Very well written!
Thank you for your kind words.
Greetings! Very helpful advice within this article! It is the little changes that produce the greatest changes. Many thanks for sharing!
Hello, thank you for your comments, much obliged.
Awesome blog! Do you have any recommendations for aspiring writers? I’m planning to start my own site soon but I’m a little lost on everything. Would you advise starting with a free platform like WordPress or go for a paid option? There are so many options out there that I’m totally overwhelmed .. Any recommendations? Thanks!
Hi, thank you for your kind words; WordPress is the way to do it! I read a lot of stuff too before starting and decided to go with WordPress; wishing you well in the future.
I’m really enjoying the theme/design of your web site. Do you ever run into any internet browser compatibility issues? A handful of my blog readers have complained about my website not working correctly in Explorer but looks great in Firefox. Do you have any suggestions to help fix this problem?
Hi, thanks for your kind words; when it comes to internet and website issues, I leave it to my tech team to deal with it. Wishing you well.
I just want to say I am just new to blogging and really savored you’re page. More than likely I’m going to bookmark your website . You absolutely have great articles and reviews. Cheers for sharing with us your web site.
Hello there, thank you for your compliments and kind words. Do bookmark and come on over to read about healthy life choices. Wishing you well.