SICKLE CELL, BLOOD EXCHANGE AND I
Not too long ago, I had to go for surgery and needed to have blood exchange before surgery. Blood exchange was something that I had never had and I was intrigued about the whole process, and wanted to tell you all about my experience. I realise that some of you might have had blood exchange before or maybe your loved one who suffers from Sickle Cell, nonetheless, it is good to write about it for some other people who are yet to have it.
Prior to my going for the blood exchange on the day in question, I previously had to go and have a blood test done, in order for them to ascertain my blood group.
On the day in question, I was told to get to the hospital for 9 am. I got there before the time said and the whole process began. It was a long day and I was very tired and in pain at the end of it all.
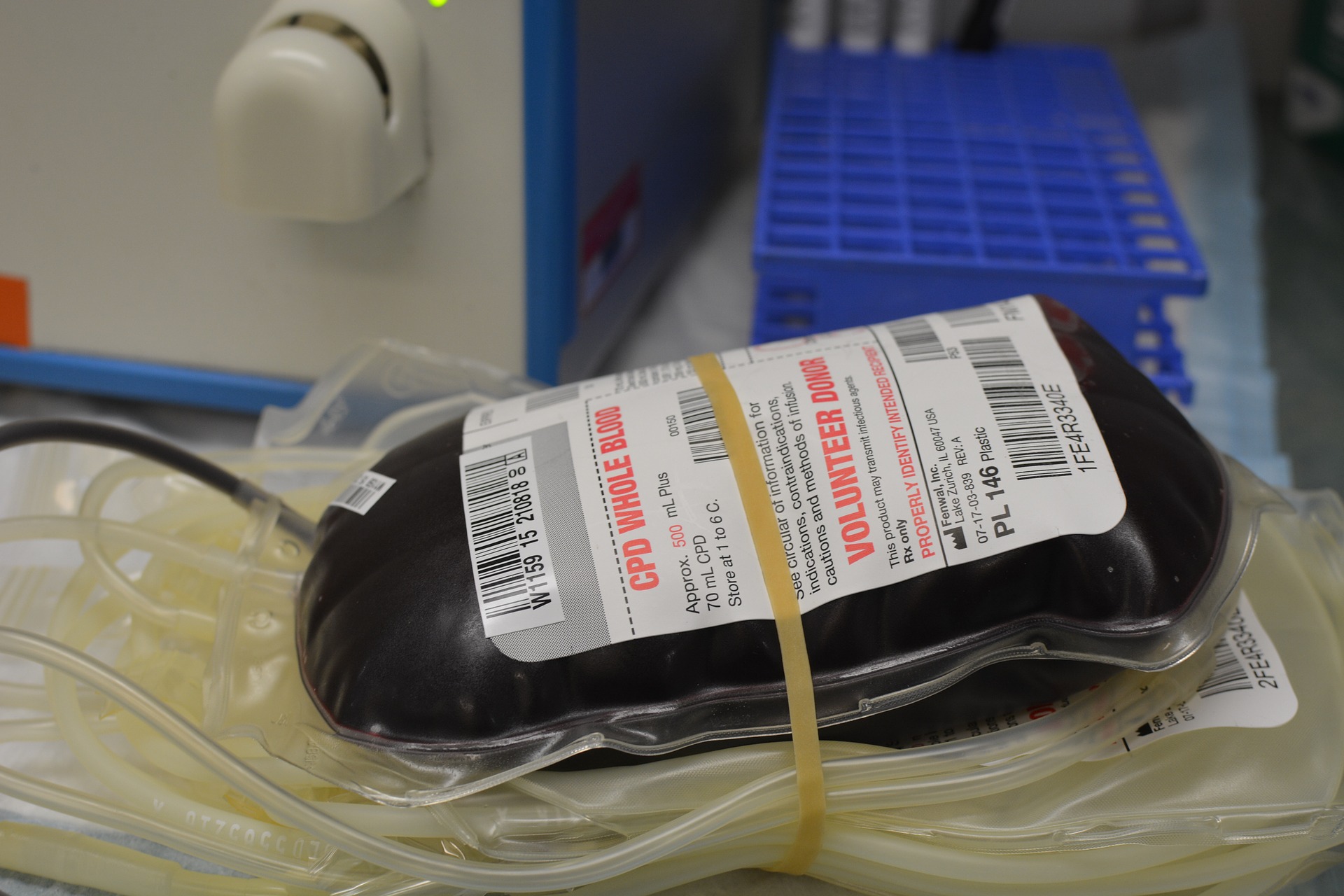
Due to the fact that I was going for surgery a few days after the blood exchange, my haematology team felt that it was important for me to have ‘good’ blood in me. The process was one of taking out my blood from one tube as another tube was feeding back into me the ‘good’ blood from the blood exchange machine.
The bit that I found painful was them trying to get a vein in order to put the cannula tube in and as the nurse could not find any veins in my hands, it was decided that this whole process would be done through my groin and men, was it painful! A femoral line, (this thing is bigger than a cannula tube) had to be inserted to my groin area.
I was also regularly monitored during the exchange (checking blood pressure, temperature, pulse and breathing rate) and asked how I was feeling.
While I was there, I found out that some people have to come for a blood exchange every 4-14 weeks! What!!! Let’s educate ourselves on blood exchange for people with sickle cell:
An exchange blood transfusion – This is a procedure that replaces sickle blood with nonsickle blood (from a donor who does not have sickle cell disease).
Why would I need an exchange blood transfusion?
This procedure might be needed in an emergency, such as for:
a complicated sickle cell crisis, such as a stroke
a chest crisis – sickling in the lungs causing breathing problems
a very painful crisis.
A routine or planned exchange transfusion may also be done in the following situations:
If you have had a stroke, repeated exchange transfusions can help reduce the risk of further strokes happening.
If your sickle cell disease is very severe, repeated exchange transfusions can help reduce the number of crises.
In pregnancy an exchange transfusion may prevent complications to you and your baby.
If you are going to have a major operation such as a hip replacement, a single exchange transfusion reduces the risk of complications from the general anaesthetic and surgery.
If you have leg ulcers exchange transfusions may aid healing.
An exchange transfusion may help in cases of severe priapism (painful erections) that have not responded to other forms of treatment or surgery.
What are the possible complications of blood transfusions?
Minor reactions – you may get a skin rash or a minor fever, for example. These can be treated easily with paracetamol and antihistamines.
Iron overload – This is common in people who receive repeated blood transfusions. When necessary, excess iron can be removed by taking medication (injections or tablets). This is much less likely when the exchange machine is used than when an exchange transfusion is performed manually.
Antibodies your blood is matched very closely with the blood of the donor (the person who donated the blood). However, it is possible to develop ‘antibodies’ against the donor blood, so you need to make the clinical staff aware of any symptoms you may be having after the transfusion (see the section on delayed transfusion reactions). These antibodies can mean that matched blood is harder to find and can take longer to prepare.
Delayed transfusion reactions
Occasionally a patient experiences a delayed transfusion reaction (where your body abnormally breaks down the blood you have been transfused), which may occur within the first two weeks of being transfused. This may cause:
severe generalised sickle cell pain/crisis
blood in the urine (red or cola colour )
feeling tired feeling short of breath
fever
localised loin / back pain.
Having a femoral line inserted
A femoral line is a cannula (tube), which is inserted into the femoral vein near the groin to give you the donor blood. It is larger than a cannula for your arm we often need to use a femoral line because we need to use a large vein for an exchange blood transfusion, especially if the blood exchange machine is used. This is called an automated exchange transfusion The femoral line is inserted by the advanced nurse practitioner or by one of the medical or specially trained nursing staff on the day unit at the hospital. You will initially attend the haematology day unit and a cannula will be inserted. You are given an injection of local anaesthetic to your groin, which is a medication used to numb the area so it is less painful. It takes about half an hour to prepare for the insertion of the femoral line, but it only takes fifteen minutes to put the line in. The line will need to be secured by a strong dressing or stitched in to stop it falling or being pulled out.
How long will the transfusion take?
The exchange blood transfusion process can take from one to four hours on the machine. This will depend on your clinical history and how much blood will be used during the procedure. However, you should expect to be in the day unit for the whole day (10am to 5pm). This is because the femoral insertion takes about 45 minutes and you should allow another hour and a half after the machine has stopped before you can leave the hospital.
What happens after the transfusion?
When the exchange is finished, blood is taken from the femoral line so we can see how much of the sickle haemoglobin is left in your blood. The femoral line is then taken out and the nurse will apply pressure with their thumb to the area for about five minutes. You will be asked to lie flat for half an hour. This is to prevent bleeding. You will finally be assessed by a nurse and, if everything is fine, you will be able to go home.
www.guysandstthomas.nhs.uk/resources/patient-information/haematology/exchange-blood-transfusion-scd.pdf






We thank God for shared knowledge and your healing.
Hello sis, much appreciated.